Documenting HIPAA forms involves ensuring that they comply with the Health Insurance Portability and Accountability Act (HIPAA) regulations, particularly concerning the privacy and security of protected health information (PHI).
Understanding the different types of HIPAA forms
To effectively document HIPAA forms, it’s essential to understand the types of forms commonly used. Each serves a specific purpose in maintaining patient confidentiality and controlling access to PHI.
- HIPAA authorization form: This form allows patients to grant permission for their PHI to be disclosed or shared with specific individuals or entities. Without authorization, healthcare providers cannot release a patient’s information except in cases allowed by HIPAA, such as treatment or billing.
- Notice of Privacy Practices (NPP): The NPP outlines how a healthcare provider will use and disclose PHI. It also informs patients about their rights regarding their health information.
- Business associate agreement (BAA): This legally binding agreement ensures that third-party service providers, or business associates, comply with HIPAA regulations when handling PHI on behalf of a covered entity.
Knowing the purpose of each form guides how it should be documented and ensures compliance at every step.
Go deeper: The different types of HIPAA forms
Ensure required elements are included
HIPAA forms must contain specific information to ensure they are valid and enforceable. Failing to include required elements could result in non-compliance and lead to potential fines or legal consequences. Here are the key components that should be included in most HIPAA forms:
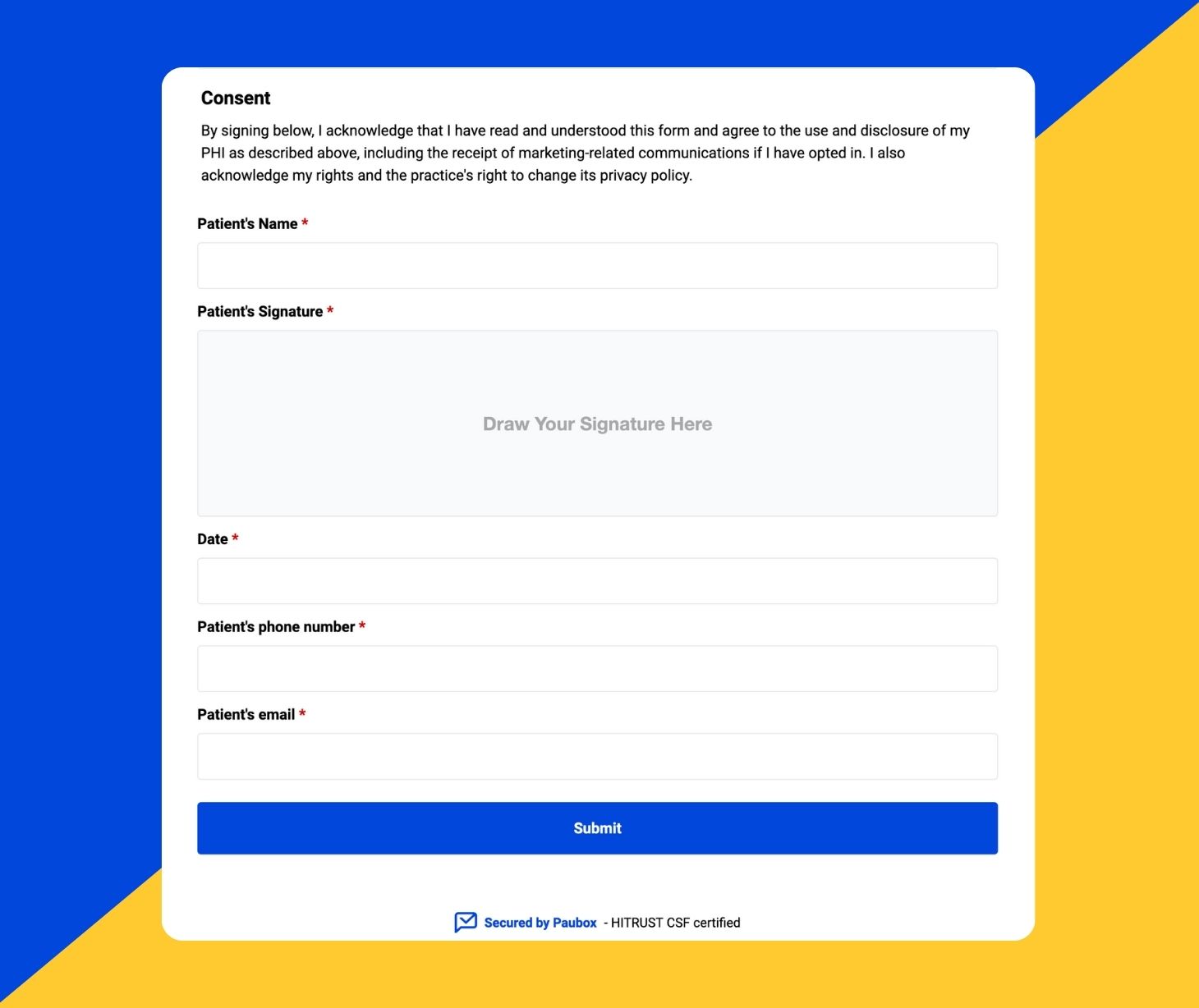
- Patient information: Include the patient’s full name, address, date of birth, and any other relevant identifiers to ensure that the form applies to the correct individual.
- Description of PHI: According to the National Institutes of Health, “the Privacy Rule defines PHI as individually identifiable health information, held or maintained by a covered entity or its business associates acting for the covered entity, that is transmitted or maintained in any form or medium (including the individually identifiable health information of non-U.S. citizens).” It includes demographic information. HIPAA forms must specify which parts of the patient’s health information will be disclosed or used. It’s important to limit the scope of the information shared to the minimum necessary to achieve the intended purpose.
- Purpose of disclosure: Indicate why the information is being disclosed or for what purpose it will be used. It could be for treatment, billing, legal purposes, or other reasons.
- Recipient information: Identify who will receive the information. Whether it’s another healthcare provider, insurance company, or business associate, this section clarifies where the data is going.
- Expiration date: State when the authorization will expire. This could be a specific date, a condition (e.g., when the treatment ends), or a set period after signing.
- Revocation clause: Patients must have the right to revoke their authorization at any time. Clearly explain how a patient can withdraw consent, along with any limitations that apply once the PHI has been disclosed.
- Signature and date: The form must be signed and dated by the patient or their legally authorized representative to be valid. Without this, the form is not enforceable.
Review for HIPAA compliance
Once the form is completed, review it for HIPAA compliance. Here are key things to check:
- Minimum Necessary Rule: Ensure that the information disclosed is the minimum necessary to accomplish the intended purpose. HIPAA mandates that only the least amount of PHI needed should be shared.
- Confidentiality measures: Make sure the process for handling, transmitting, and storing PHI is secure, whether the form is paper-based or electronic. For electronic forms, encryption and secure access protocols should be in place.
- Patient rights: Confirm that the form provides information about the patient’s rights, including the right to access, amend, and request restrictions on their health information.
The review process helps catch any potential errors or omissions that could lead to non-compliance, helping to prevent fines, breaches, and legal complications.
Use version control and track updates
Healthcare laws and regulations change over time, and your HIPAA forms must stay current. Documenting version control and updates ensures compliance with the most up-to-date standards.
- Tracking versions: Keep a log of when HIPAA forms were created, updated, or revised. This ensures that all staff and patients are use the latest version of the form.
- Making updates: When changes to the form are necessary, whether due to regulatory changes or improvements in internal procedures, clearly document the changes and the reason for the update.
Having a strong version control system helps prevent outdated forms from being used, which could lead to inadvertent HIPAA violations.
Electronic vs. paper HIPAA forms
Many healthcare organizations have shifted to electronic HIPAA forms, but some still rely on paper-based systems. Studies show that the COVID-19 pandemic dramatically accelerated the adoption of digital technologies, especially in healthcare, where health tech has been developing for decades. “COVID-19 testing, contact tracing, other diagnosis programs needed this change.”
Each method has its own documentation and security requirements:
- Electronic forms: If you use electronic HIPAA forms, they must comply with the HIPAA Security Rule, which sets standards for protecting electronic PHI (ePHI). This includes encryption, secure user authentication, and regular audits of access logs.
- Paper forms: Paper forms should be stored securely, typically in locked file cabinets or secure areas with limited access. Include clear policies for retrieving, copying, and destroying paper forms.
Whether using electronic or paper forms, healthcare organizations must have detailed policies in place that dictate how these forms are handled to ensure HIPAA compliance.
Retain forms for the required period
HIPAA requires that covered entities retain HIPAA-related documentation for a minimum of six years from the date of creation or the last effective date, whichever is later.
Ensure that forms are stored securely for the required time and that they are readily accessible in case of audits or legal inquiries.
Conduct regular audits
Regular internal audits of your HIPAA forms and documentation processes help ensure that your organization remains compliant. Audits should focus on:
- Form completeness: Verify that all required fields are filled out correctly.
- Secure storage: Ensure that forms—whether electronic or paper—are stored securely.
- Access controls: Review who has access to HIPAA forms and ensure it is limited to authorized personnel.
Document the results of these audits, as well as any corrective actions taken in response to identified issues.
Learn more: How to conduct a HIPAA compliance audit
Train employees on documentation procedures
All employees who handle PHI must be trained on documenting HIPAA forms correctly. Training should cover:
- How to complete forms: Educate staff on how to correctly fill out forms to avoid errors or missing information.
- Security protocols: Train employees on the importance of securing both paper and electronic forms.
- Patient rights: Ensure employees understand how to explain HIPAA forms and patient rights to individuals who have questions.
Document all training sessions and keep records for compliance purposes.
Go deeper:
- Collect patient data securely with Paubox Forms
- Guidelines for HIPAA compliant documentation and record retention
FAQs
What security measures are required for electronic HIPAA forms?
For electronic HIPAA forms, organizations must follow HIPAA’s Security Rule, which requires:
- Encryption: To protect data when stored or transmitted.
- Access controls: Ensure that only authorized personnel can view or edit the PHI.
- Audit trails: To track who accessed the data and when, ensuring accountability.
Can a patient revoke their authorization after signing a HIPAA form?
Yes, patients have the right to revoke their authorization at any time. However, the revocation is only effective moving forward and does not apply to information already disclosed based on the original authorization.
What happens if a healthcare organization fails to properly document HIPAA forms?
Failure to properly document and secure HIPAA forms can lead to significant consequences, including:
- Fines: HIPAA violations can result in fines ranging from $141 to $71,162 per violation, depending on the level of negligence.
- Legal action: Patients can file lawsuits if their PHI is mishandled.
- Reputation damage: Breaches in HIPAA compliance can damage an organization's reputation and erode patient trust.
Subscribe to Paubox Weekly
Every Friday we'll bring you the most important news from Paubox. Our aim is to make you smarter, faster.